Population Health Part 1
Intro to pop health, measures, determinants, SDoH and behavioral health factors
OK - I have a lot of notes on Pop Health stuff, so I’m going to try to break it up into a few smaller posts as I go along so I can keep publishing. This is going to be a pretty high level intro to some terms and ideas. As always, I’ll try to include a lot of links to more robust resources along the way.
In my next posts on these topics, I’ll start introducing some tools for looking at population health.
Then, I’ll do a more practical level walk through of how pop health works in practice with VBC models
What is Population Health?
I like this definition of population health that I found in this paper about population health terms:
“the health outcomes of a group of individuals, including the distribution of such outcomes within the group” (Kindig and Stoddart 2003, 381)
So, it’s fundamentally about measuring health among a specific group of people. Obviously, people use this data for a lot of applications. It’s key to implementing a value-based care practice, public health interventions, etc, but at it’s core it’s about measurement.
How is it different than public health?
From the same paper, here’s the definition of public health:
“Public health: (1) Activities that a society undertakes to assure the conditions in which people can be healthy. These include organized community efforts to prevent, identify, and counter threats to the health of the public (Turnock 2004). (2) What we do as a society collectively to assure conditions in which people can be healthy (IOM 1988).”
So public health is about what we do as communities and governments to improve health and to fight or prevent disease. Measurement is part of this, but it’s mostly about policy and interventions. It’s also not so much about how you set up a clinical practice, which population health implementations can be used for.
Kindig’s Model
David A. Kindig is one of the leaders of the population health field. I’m going to be using a lot of the terms from his model, which is visually illustrated below.
His blog can be found here, and it’s a great resource for everything population health.
Weighting the different determinants is an ongoing discussion in the literature, but Kindig mentions the County Health Rankings (we’ll talk about this resource in more detail in a future post) weighting system in his blog:
In the MATCH County Health Rankings, health care is weighted 20%, behaviors 30%, the social environment 40%, and the physical environment 10%. An explanation of the process used to assign these particular weights is available.

Key Population Health Outcome Measures
The following are measures to be familiar with in discussions of population health. These are very well explained in this paper (Health Indicators Related to Disease, Death, and Reproduction), which also contains a lot more detail for those who are interested.
Mortality
Infant mortality
Life Expectancy
Child mortality
Morbidity
Incidence: proportion of individuals who start the time period well, but end up developing a disease
Prevalence: proportion of individuals with a disease or condition within a given time period
Quality of Life
A pretty broad concept encompassing how good ones’s life is at a given time
Quality adjusted life year- a measure of quality where 0 means a ‘health state equivalent to death’ and 1 means optimal health.
Disability
Something that reduces ones ability to function in society
Things like mobility impairment, sensory impairment, etc.
Disparities
Disparities are differences or variations in outcomes by rank, amount or quality between sub-groups of the population. Disparities can be measured across things like
Race
Ethnicity
Geography
Gender
I hope we can delve deeper into disparities later. In the meantime, this paper by the Kaiser Family Foundation is a great intro.
Determinants
A factor that brings about a change in health condition or other characteristic that we care about.
In population we usually talk about the following things being determinants of health outcomes:
Healthcare access, availability or use
Behavior
Social environment
Physical environment
Genetics
In this post, we’ll look at social, physical and behavioral determinants.
We’ll talk more about the design of the health care system in a lot more detail in later posts.
Genetics is a super complex topic but we’ll just leave it pretty simple here: Some people are genetically predisposed to certain conditions, diseases and health outcomes. Those factors are not easily influenced by a population health approach, so we won’t spend a ton of time on them.
Risk Factors
An overlapping and alternative way of looking at determinants of health is to consider Risk Factors for specific common conditions (heart disease, cancer, diabetes, etc.)
Risk factors are conditions or behaviors that increase the likelihood of getting a disease or injury. These are usually talked about as specific to a given condition, like the risk factors for heart disease. However, risk factors often coexist and interact with one another. Risk factors for many conditions are overlapping.
Some risk factor categories include:
Dietary behavior- could be either personal choice or access to healthy food
Physical inactivity
Sexual behavior
Tobacco use
Drug or alcohol use
Environmental conditions
Unsafe neighborhood
Environmental hazards
Eg. air quality, or unsafe conditions at work
Demographics
Age
Geography
Obesity
Insurance status
Blood Pressure
Cultural stigmas
eg. against seeing a doctor
Genetics
Diet
Safety measures
eg. wearing a seatbelt
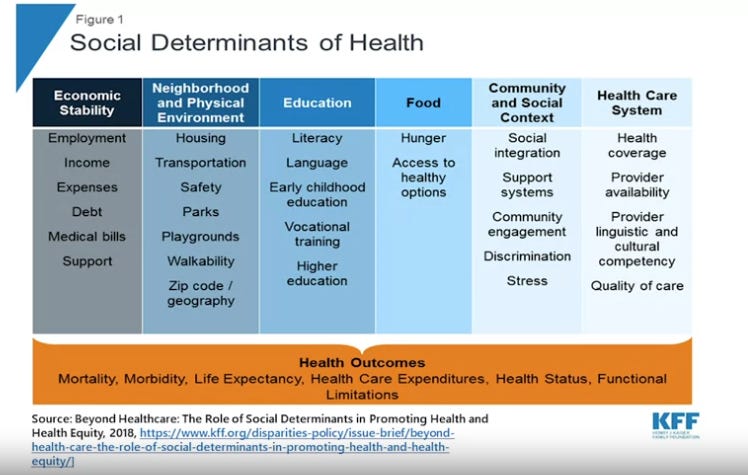
Social Determinants of Health (SDoH)
The Social Determinants of Health are all the factors about the places and conditions in which people live that affect their health. Talking about SDoHs acknowledges that much of what impacts peoples’ health happens outside of the health care system.
Kaiser Family Foundation framework is a good primer for talking about these factors.
This graphic tells you a little about what some of these factors are.
Another related term you might here in connection with SDoH is:
HRSN - Health Related Social Needs
This is closely tied to the CMS’s HRSN survey, which helps clinical and public health practitioners determine individuals’ needs with regards to:
Housing instability
Food insecurity
Transportation problems
Utility help needs
Interpersonal Safety
Financial strain
Employment
Family and Community support
Education
Physical Activity
Substance Use
Mental Health
Disabilities
Behavioral Health
Behavioral Health is actions that people take that affect their mental or physical health.
Mental Health
Mental health factors include risk for depression, anxiety disorders or suicide
Substance Use Disorders
Substance use disorders are an important set of disorders that are related to behavior. They are a cluster of cognitive, behavioral, and physiological symptoms that indicate that someone continues to use a certain substance despite significant negative effects on their lives and the lives of those around them.
Physical Determinants of Health
These are the factors within the physical environment that affect health in measurable ways. Some factors here are:
Cleanliness of air
Cleanliness of water
Healthy workplaces
Safe housing
Wrapping up
There’s a ton of stuff that follows on from what we’ve covered here, which we’ll get to soon.
For now, you should note that Population Health is about measuring health outcomes for a group of people and the things that we measure are things that determine health (social, clinical, physical, behavioral, and genetic) and overlapping risk factors for specific conditions. Health within a population can also vary based on things like demographics, race, ethnicity, socio-economic status and other things.
We’ll talk about how to measure this stuff and what to do with it in the next posts.