Population Health 3
Pop Health Management: Chronic Conditions, Risk Levels and Strategies for different patient types
Population Health Management
Managing the health of the population means knowing who your population is and what their health is like, and we’ve discussed ways of finding that out in parts 1 and 2
Here we’re going to look at the most common chronic diseases, managing those diseases and the most common risk factors for those diseases and how to manage them so they don’t make diseases worse.
That will lead us to looking at the whole population to assess the number of people with diseases that put them at risk for more acute and dangerous episodes that might lead to hospitalization or death, and how many people are relatively healthy.
That will lead us to a discussion of risk levels and the population health pyramid.
Then we will revisit value based care which suggests preventative interventions for different kinds of people in the population.
Chronic Disease
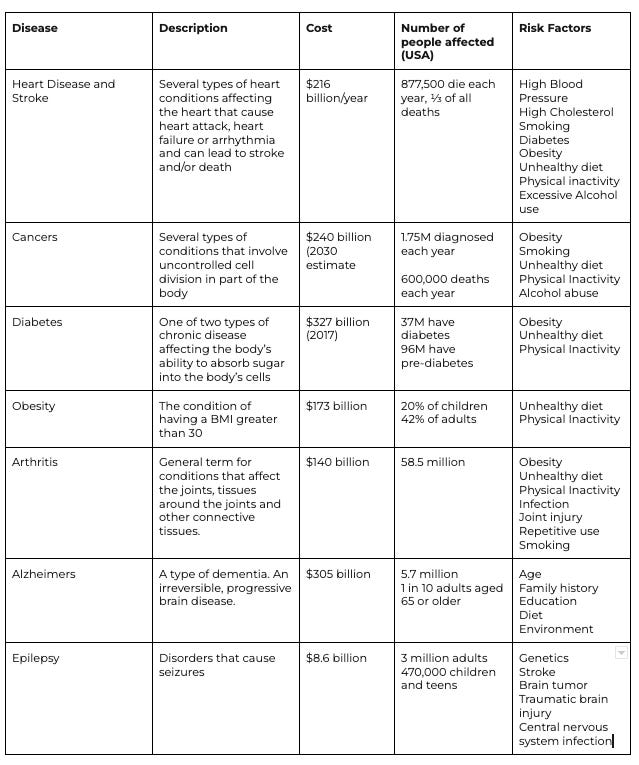
Let’s look at the most common chronic diseases. This information is taken from the CDC’s Chronic Disease site
Collectively, these diseases kill millions of Americans each year and cost trillions of dollars to the American economy.
However, many can be well managed, partially reversed or prevented with the right kind of care. Managing chronic diseases well can lengthen the lives of those affected, improve their quality of life, and in some cases reverse the symptoms of the disease.
Population health management gives us some tools for approaching populations that have large numbers of people with chronic disease.
Common Risk factors
As you can see in the table below, many chronic diseases share the same risk factors. Addressing these risk factors for the population can lower the rates of chronic disease over time.
The CDC calls out Three common risk factors:
Cigarette smoking - Still the leading cause of preventable death in the US! 16 million Americans have a disease caused by smoking.
Physical inactivity - A risk factor for heart disease, diabetes, cancers and obesity. Increasing physical activity for a population can improve outcomes quite a bit at the margin
Excessive Alcohol use - In addition to being a risk factor to many of the chronic conditions above, excessive drinking can cause accidental deaths and injuries, and is implicated in a lot of violent crime. It’s estimated to be responsible for 140,000 deaths per year
Other risk factors I would call out are:
Age - most, if not all, chronic conditions get more prevalent with age
Other substance abuse - this is a growing problem, with lives being increasingly affected by a number of other drugs like opioids, fentanyl and heroin
Loneliness - lack of connection is a growing problem in the US.
Social and Environmental determinants - we talked about these quite a bit in the last couple posts, but they are a substantial determinant not just of general health but of chronic diseases.
Addressing the top chronic conditions and top risk factors across a population can have dramatic affects on outcomes.
Next, we’ll look at an approach to organizing population by risk and how to approach each risk segment.
Risk and the Pop Health Pyramid
This post is going to gloss over one somewhat difficult problem and move on to looking at risk levels and categories, but I do want to at least name that problem and define it.
It’s the problem of attribution - knowing which patients your health care organization is responsible for. In an ideal case, you can define this within a contract with a payer, but sometimes it’s not clear.
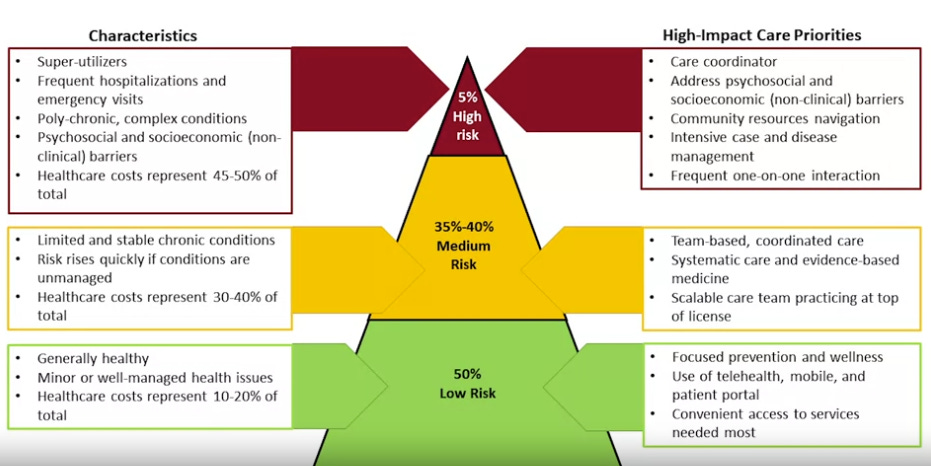
But, once the population has been identified, it should be segmented by 3 risk categories: high medium, low.
We need to develop strategies for each of the three risk groups, and each requires different model of care.
Low - Roughly 50% of population. They are Healthy or have a well managed chronic condition. Their socio-economic status is stable. For this group we can focus on patient portals and telemedicine, and give patients tool to manage their own health.
Medium - About 35% of population. They might have one or more mild chronic conditions and live around the edges of SES determinants. If not addressed, risk factors could push them into the high risk category. Annually about 18% of the medium risk population becomes high risk. Medium risk patients might be given a home based care plan, patient and caregiver education, and opportunities to connect with peer groups and mentors.
High - About 5% of population but responsible for 50% of healthcare cost, high risk patients are sometimes called ‘superutilizers’. They have at least complex chronic condition, co-morbidities, psychosocial needs, and/or unstable SES. They might frequently utilize hospitals and emergency rooms. Patient care should be coordinated and managed through a care team. High-touch, in home care is ideal for these patients. Likely high touch care like this will still reduce the overall cost of treating the patient, as it will keep them out of hospitals and emergency departments.
There are estimates that $240 of prevention can save $1000 in reactive treatments (here’s a good paper on the savings).
(https://www.coursera.org/learn/pop-health/lecture/tAjKj/the-population-health-pyramid)
An alternative triangle
There are alterntative triangles with different allocations for high, medium and low risk patients, for example this Iron Triangle, mathematical model for assessing pop health risk.
Population health management and value based care.
86% of expenses are for chronic conditions.
Determining risk
In order to categorize the population, you will need some data. Often payers will make some kind of risk segmentation recommendation. You can also analyze claims data, work with providers, community groups that collect the data or tech aggregators for your population to see which patients might fall into which category as defined above.
This can be combined with an approach of having providers help categorize and label patient risk levels within the EMR.
It can be a time consuming process to go over the patient list and categorize patients, but it can yield much better out comes.
Drivers of risk
For medium and high risk patients, it can be helpful to identify the drivers and help to address them. They could be just access to treatment, that can be addressed by home-based care. Or they could involve creative planning to address social and environmental determinants.
When looking at your population, you can ask yourself the following questions to begin to put together care plans:
Who are riskiest patients?
Which patients likely to become risky in the future
Why are they risky?
What interventions can we make to address root cause?
Ideally for the ones determined to be most risky, you’d want to collect data on their:
health behaviors
health statues
clinical care access
use and quality of available services
social and economic factors
Tying back to value-based care
This type of population health management works hand in hand with value-based care. Under VBC plans, providers are rewarded for:
Decreased ER visits
Decreased readmissions
Increased medication adherence
Increased adherence to HEDIS measures
Developing a population health management strategy within the framework of a VBC contract should hopefully result in financial up side for providers.
Resources:
Berkowitz, S.A., Baggett, T.P., & Edwards, S.T. (2019). Addressing Health-Related Social Needs: Value-Based Care or Values-Based Care? Journal of General Internal Medicine, 34(9), 1916–1918. doi: 10.1007/s11606-019-05087-3. https://link.springer.com/article/10.1007/s11606-019-05087-3 This article provides a framework for considering health-related social needs such as food insecurity, housing instability, and lack of transportation.
Dimock, M. (2019). Defining generations: Where Millennials end and Generation Z begins. From the Pew Research Center. https://www.pewresearch.org/fact-tank/2019/01/17/where-millennials-end-and-generation-z-begins/ This article describes many factors related to generational differences and changes in views over time of different cohorts. Harvard Pilgrim Health Care. The Right Health Care Options for Your Client's Multigenerational Workplace. https://www.harvardpilgrim.org/hapiguide/generation-employer-plans/ This article provides a wealth of information about the five generations in the workplace, how they get information, and how they prefer to receive healthcare. Humana. (2019)
Onie, R. (2012). What If Our Healthcare System Kept Us Healthy? TEDMed talk. https://www.ted.com/talks/rebecca_onie_what_if_our_health_care_system_kept_us_healthy Rebecca Onie, co-founder of Health Leads and the Health Initiative, shares a TEDMed talk